- July 18, 2024
- by Shalini Murmu
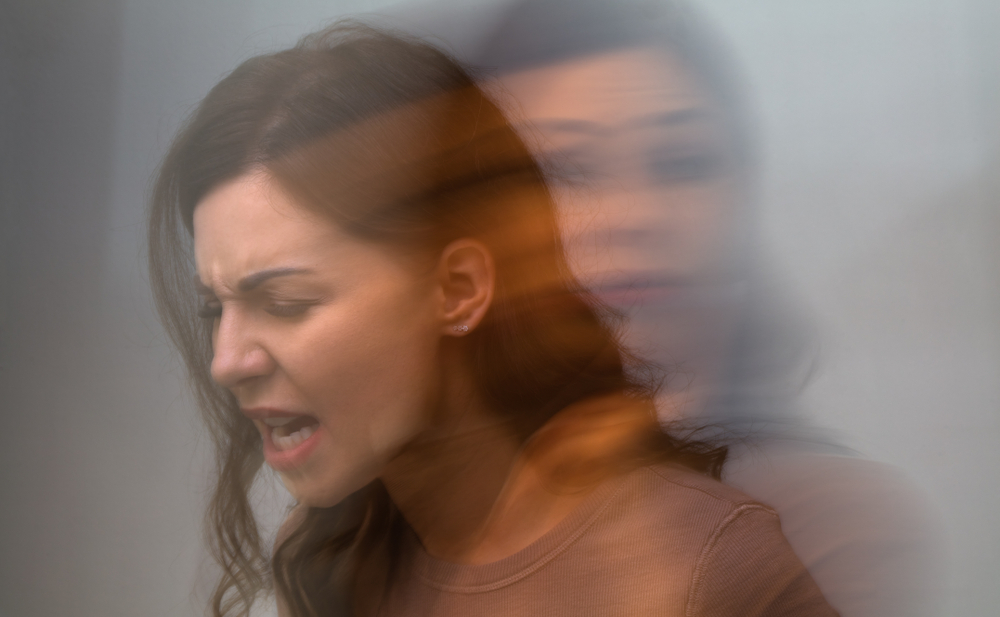
- Schizoaffective Disorder
Understanding mental health disorders is a complex and often misunderstood subject that encompasses various facets. These conditions can present themselves on a broad spectrum, exhibiting different levels of severity and unique manifestations in each person. Amidst these complex conditions are schizophrenia and schizoaffective disorder, both sharing some similarities but also possessing distinct variations that are pivotal in precise diagnosis and the efficacy of treatment.
What Is Schizophrenia?
Schizophrenia, a widely recognized yet often misunderstood mental health disorder, is a chronic and severe condition that significantly influences an individual’s cognition, emotions, and behaviors. Those afflicted with schizophrenia may exhibit symptoms that make them appear disconnected from reality, causing distress not only to themselves but also to their close ones. According to DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition), the diagnosis of schizophrenia relies on the presence of two or more specific symptoms persisting for a significant duration within a one-month timeframe, with at least one of these symptoms:
- Delusions
- Hallucinations
- Disorganized speech
- Grossly disorganized or catatonic behavior
- Negative symptoms (e.g., diminished emotional expression)
Common Misconceptions
Despite widespread awareness, various misconceptions about the disorder continue to circulate. A common fallacy is the notion that schizophrenia entails having multiple personalities, which in reality is different from dissociative identity disorder (formerly referred to as multiple personality disorder). Another prevalent misconception revolves around the belief that a schizophrenic person is inherently prone to violence, whereas statistics actually indicate that they are more susceptible to being victims of violence rather than being perpetrators themselves.
Among the various types of hallucinations observed in schizophrenia, hearing voices stands out as the most prevalent one. Similarly, delusions form another category of positive symptoms, involving strong convictions that lack grounding in reality. An individual experiencing delusions may firmly believe in possessing extraordinary abilities or facing persecution from invisible entities.
On the other hand, negative symptoms denote a reduction or absence of typical functions, posing significant challenges to daily functioning. One such negative symptom is affective flattening, characterized by a diminished range and intensity of emotional displays. This may appear as a lack of facial expressions or an avoidance of eye contact, hindering interpersonal interactions. Another negative symptom, alogia, pertains to a decrease in speech output, leading to difficulties in engaging in conversations. Individuals exhibiting alogia might provide brief, unelaborated responses to inquiries, impacting communication dynamics.
Cognitive Symptoms
Cognitive symptoms are related to thought processes. They can be subtle but are crucial for understanding the overall impact of schizophrenia:
- Disorganized Thinking: This can manifest as difficulty organizing thoughts or connecting them logically. Conversations may be hard to follow, and the person might jump from one topic to another without a clear connection.
- Memory Issues: These can include problems with working memory, making it hard to keep information in mind while using it. This affects daily activities like following instructions or remembering tasks.
Treatment and Management
1. Medication (Antipsychotics)
Effective management and treatment of schizophrenia and schizoaffective disorder typically require a comprehensive approach that includes medication, psychotherapy, and a strong support system. The cornerstone of medical intervention for these conditions is the use of antipsychotic drugs. These medications function by modifying the influence of neurotransmitters in the brain, particularly dopamine, to aid in alleviating symptoms.
- First-generation Antipsychotics: These are older medications, such as haloperidol and chlorpromazine, which can be effective but often come with significant side effects like tardive dyskinesia.
- Second-generation Antipsychotics: Newer medications, such as risperidone, olanzapine, and lumateperone, tend to have fewer side effects and are often preferred. They target a broader range of symptoms, including both positive and negative symptoms of schizophrenia.
It is important to understand that the process of finding the right medication for each person can be a journey filled with trial and error. Regular monitoring and supervision by a healthcare provider can help manage any potential side effects and make necessary adjustments to the dosage as required.
2. Psychotherapy
Medication alone isn’t sufficient when it comes to the management of conditions such as schizophrenia or schizoaffective disorder. Along with Psychotherapy, signs of schizophrenia are better managed.
CBT is a type of therapy that supports patients in recognizing and adjusting distorted thoughts and behaviors. This kind of treatment has displayed extraordinary effectiveness in reducing the impact of hallucinations and delusions experienced by affected people.
Family Therapy, another valuable approach, involves the participation of family members in the treatment process. This not just offers additional support to the patient but also helps family members gain a deeper understanding of the disorder and learn how to best support their loved one who is struggling with it.
Furthermore, Social Skills Training is an essential component of therapy aimed at helping individuals enhance their social interactions and daily functioning. These aspects are often significantly affected by the disorder, making this type of training crucial for individuals striving to improve their overall well-being.
Support Groups and Rehabilitation
Support systems and rehabilitation programs play a crucial role in assisting individuals diagnosed with mental health conditions to lead more fulfilling and meaningful lives. These programs encompass a variety of components that are designed to cater to the specific needs of those struggling with these mental health conditions:
- Residential Treatment Programs: These provide a structured environment where patients can receive intensive treatment and support. They are particularly beneficial for those with severe symptoms or who are transitioning from hospital care.
- Vocational Rehabilitation: This helps one develop job skills and find employment, which can improve self-esteem and independence.
- Peer Support Groups: Connecting with others who have similar experiences can reduce feelings of isolation and provide valuable insights and encouragement.
Schizoaffective Disorder
Schizoaffective disorder involves a combination of symptoms from schizophrenia and mood disorders. Dealing with a complex condition like this involves challenges in terms of both diagnosis and treatment, given that it exhibits symptoms of both schizophrenia and mood disorders.
As outlined in the DSM-5, schizoaffective disorder is defined by a continuous period of illness where there is a significant mood episode (either major depressive or manic) alongside symptoms that align with Criterion A for schizophrenia. Furthermore, there must be a minimum of two weeks of psychotic symptoms present without major mood symptoms being predominant.
One common misunderstanding regarding schizoaffective disorder is the belief that it is merely a milder version of schizophrenia, which is not true. Although there are similarities in symptoms with schizophrenia, schizoaffective disorder also encompasses notable mood disorder symptoms, distinguishing it as a separate and unique condition. Another misconception is that schizoaffective disorder is rare; however, it is actually quite common and often overlooked or misidentified.
Diagnostic Criteria
The DSM-5 outlines specific criteria for diagnosing schizoaffective disorder. Key points include:
- A major mood episode (depressive or manic) concurrent with symptoms meeting Criterion A for schizophrenia.
- Delusions or hallucinations for two or more weeks in the absence of a major mood episode during the lifetime duration of the illness.
- Symptoms that are not attributable to the effects of a substance or another medical condition.
Medication And Therapy
The way medication and therapy are approached varies for schizophrenia and schizoaffective disorder because of their different symptom profiles. When treating schizoaffective disorder, medications like antipsychotics are often combined with mood stabilizers such as lithium or valproate, as well as antidepressants depending on the type of mood symptoms present.
While undergoing psychotherapy, such as cognitive behavioral therapy (CBT), can be beneficial for both disorders, it must be tailored to specifically address the distinctive symptoms of schizoaffective disorder. Treatment plans may involve a more varied medication routine and incorporating strategies for managing mood within therapy sessions. Customized treatment plans make sure that each aspect of the disorder is managed effectively, offering a more holistic approach to treatment.
Comparative Recovery Rates
Recovery rates can differ between schizophrenia and schizoaffective disorder because of how symptoms present and how well they respond to treatment. Typically, individuals with schizoaffective disorder may have a more favorable prognosis compared to those with schizophrenia, particularly if their mood symptoms are effectively managed. While dealing with mood symptoms can be challenging, they may respond better to treatment than the more persistent psychotic symptoms seen in schizophrenia.
It’s worth noting that the journey to recovery is unique to each individual. Some people with schizophrenia experience significant progress and live fulfilling lives, particularly with prompt intervention and consistent treatment. Similarly, those with schizoaffective disorder may face fluctuations in their condition, necessitating ongoing adjustments to their treatment plans.
Impact On Quality of Life
The impact of schizophrenia and schizoaffective disorder on quality of life is deep and complex. Schizophrenia can greatly affect social and work life due to ongoing psychotic symptoms and cognitive challenges. When early signs like social withdrawal or decline in performance are ignored, they can significantly change a person’s future.
Quality of life is also impacted by schizoaffective disorder, which can have periods of stability mixed with severe symptoms. Dealing with both psychotic and mood symptoms can be tough due to the unpredictability of the condition.
Support systems, like family, peers, and residential treatment, are crucial for both disorders. Many individuals manage their symptoms well with medication, therapy, and strong support networks, leading fulfilling lives.
Know What You Are Going Through With North America Behavioral Health Services
Have you watched the mentioned symptoms yet not sure what you or your loved one is struggling with? Don’t worry, North America Behavioral Health Services is here to help. We offer expert care for early diagnosis and guide you to leading mental health facilities with treatment options that align with your needs. Recovery is not only possible but also within reach. There is absolutely no shame in seeking mental health assistance. The sooner you seek help, the better the outcomes. Connect with us today to learn more and take the first step towards a healthier, happier future.