- May 13, 2025
- by Shalini Murmu
- Mental Health
PMS and PMDD are cyclical disorders associated with the luteal phase of the menstrual cycle. An important fraction of women of reproductive age undergo PMS, with an estimated 30–50% admitting to having at least mild symptoms. PMS often presents itself through a range of physical symptoms like abdominal bloating, tenderness in the breasts, headaches, and a general feeling of fatigue, in addition to emotional and behavioral reactions such as increased irritability, anxiety, low mood, and trouble maintaining concentration, which usually arise 7 to 10 days ahead of the menstrual cycle and diminish once menstruation starts.
PMDD is a more severe and debilitating variant of PMS that the DSM-5 categorizes as a depressive disorder; it necessitates the presence of at least five out of eleven symptoms in the final week leading up to menstruation, including a core mood symptom (for instance, significant irritability, depression, or anxiety). Approximately 3–8% of women globally are affected by PMDD. Those suffering from PMDD endure extreme mood fluctuations and significant impairment, with research indicating that they experience ~4 times the rate of suicidal thoughts and ~7 times the rate of attempts compared to those without PMDD.
Conversely, while PMS (without satisfying the full criteria for PMDD) is prevalent, it tends to be less disruptive, although it is still associated with increased levels of anxiety and self-reported cognitive difficulties.
Physiological and Psychological Changes
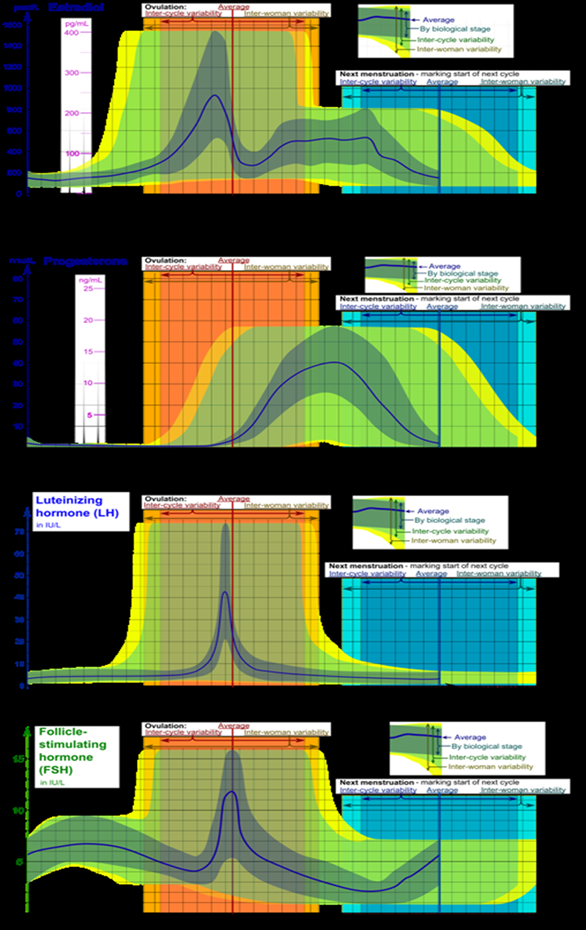
Premenstrual symptoms stem from normal hormonal fluctuations, but they arise due to atypical sensitivity to these hormones. Over the course of the menstrual cycle, estrogen and progesterone levels, along with their regulators LH and FSH, fluctuate (see diagram below) – every woman has a peak in estradiol midway through and experiences a rise in progesterone during the luteal phase. In instances of PMS and PMDD, the quick upswing of progesterone in the luteal phase, succeeded by its decline and its neurosteroid metabolite allopregnanolone, seems to have a significant impact on the onset of symptoms.
Allopregnanolone serves as a powerful modulator of GABA_A receptors, and research indicates that women experiencing PMS or PMDD might develop neurobiological tolerance or altered sensitivity to GABA during the luteal phase. The levels of reproductive hormones themselves remain normal; instead, those with PMS or PMDD exhibit an exaggerated central nervous system response to these cyclical fluctuations. Other mechanisms that may be involved include serotonergic dysregulation (with PMDD often showing improvement through serotonin reuptake inhibitors), estrogen-related genetic variations (such as ESR1), and interactions between neuroinflammation and stress.
Recent reviews have pointed out elevated inflammatory markers (like IL-6, TNF-α, and CRP) and heightened perceived stress levels in cases of severe PMS or PMDD, establishing a connection between HPA-axis stress responses and the severity of menstrual symptoms.
Figure: Typical fluctuations in menstrual cycle hormones (estradiol, progesterone, LH, FSH). In PMS/PMDD, the rise and fall of luteal progesterone (along with allopregnanolone) (as illustrated by the green curve) is believed to trigger symptoms in susceptible women.
Psychological/Mood changes: During the luteal phase, women experiencing PMS or PMDD frequently encounter irritability, anxiety, and mood fluctuations that can be either depressed or unstable. These symptoms are often tearfulness, anger, feelings of being “overwhelmed,” social withdrawal, and an increased sensitivity to rejection. Commonly experienced are cognitive challenges like issues with focus, forgetfulness, or ‘brain fog’. On a physiological level, PMS/PMDD may lead to breast tenderness, bloating, headaches, muscle aches, changes in sleep patterns (whether hypersomnia or insomnia), and changes in appetite. In PMDD, emotional symptoms are particularly pronounced and can lead to significant impairment. In contrast, “mild PMS” generally results in only minimal discomfort.
Mental Health Implications
Women experiencing PMS, particularly those with PMDD, exhibit higher rates of psychiatric comorbidities. Even in the absence of PMDD, PMS frequently coincides with mood and anxiety disorders. Research indicates that PMS is often linked with major depression, dysthymia, panic disorder, or generalized anxiety disorder (GAD). PMDD, in particular, poses a significant burden: women with PMDD experience impairments comparable to those seen in major depression.
A meta-analysis revealed that the risk of suicidal ideation associated with PMDD is approximately four times greater, and the risk of suicide attempts is around seven times higher (adjusted odds ratios) when compared to women who do not have PMDD. Anxiety and irritability during the premenstrual phase are nearly ubiquitous among those with PMDD. In practice, about 40% of women seeking treatment for PMDD actually present with a premenstrual exacerbation of another disorder, such as bipolar disorder or persistent depression, highlighting the importance of thorough evaluation.
Cognitively, some women report difficulties with attention and memory prior to menstruation. Objective studies yield mixed results: a recent review indicates that cognitive performance fluctuates significantly throughout the menstrual cycle, making it unclear whether any deficits arise from hormonal effects or are secondary to mood disturbances. Behaviorally, women often experience heightened fatigue during the luteal phase, which may impact their daily functioning.
Management Strategies
The effective management of PMS/PMDD employs a multimodal approach, customized based on the severity of symptoms (mild, moderate, or severe). The 2023 ACOG guideline, along with various reviews, supports a strategy that combines lifestyle changes, psychotherapy, and pharmacological treatments. Key evidence-based approaches include:
- Lifestyle and Self-care: Engaging in regular aerobic exercise (≥150 minutes per week) significantly alleviates both physical and emotional symptoms associated with PMS. Techniques that integrate mind and body, including yoga, meditation, and mindfulness, are beneficial for alleviating anxiety and boosting mood. Following a healthy and balanced diet (for instance, a Mediterranean diet) offers protective benefits: a “Western” diet, characterized by high levels of processed foods and sugar/salt, correlates with an increased risk of PMS, while diets abundant in fruits, vegetables, lean proteins, and whole grains are linked to milder symptoms. Reducing the intake of caffeine, refined sugars, and salt may also be advantageous. It is advisable to prioritize adequate sleep and effective stress management.
- Nutritional Supplements: Taking calcium supplements at around 1,200 mg each day has significant backing from randomized controlled trials that show a reduction in the severity of PMS. Supplementation with vitamin D and magnesium may also provide benefits for certain women. Taking Vitamin B6, specifically pyridoxine, at doses of up to 50 mg daily can lead to slight enhancements in mood. Chasteberry (Vitex agnus-castus) is supported by clinical trials (featuring two high-quality RCTs) for easing PMS discomfort. Conversely, evening primrose oil and St. John’s Wort have not demonstrated clear benefits in research studies. Consulting with a healthcare provider is recommended for women considering supplements, as there can be side effects or interactions involved.
- Psychotherapy: For managing PMS/PMDD-related mental health conditions, cognitive-behavioral therapy (CBT) has demonstrated its effectiveness. Several RCTs, along with their meta-analyses, demonstrate that cognitive behavioral therapy is quite effective in mitigating anxiety, depression, and the general symptom burden. A recent comprehensive study found that the size of the effect from CBT on PMS symptoms was similar (small to moderate) to that of antidepressants. Mindfulness-based stress reduction or cognitive-behavioral therapy (MCBT) also yields positive results. CBT can be administered in individual or group settings (including online) and is particularly suitable for mild to moderate cases or for individuals hesitant about the use of medications. Psychoeducation by itself has modest benefits and is frequently integrated into CBT programs.
- Pharmacotherapy: For those experiencing moderate to severe PMS/PMDD, the recommended first-line approach consists of antidepressants, particularly SSRIs. Research indicates that fluoxetine, sertraline, paroxetine, or escitalopram can significantly lessen mood disturbances and bodily sensations. SSRIs can be prescribed continuously or exclusively during the luteal phase (starting approximately 14 days prior to menstruation); both methods are effective, although some data suggest a preference for continuous dosing. Symptom-onset dosing (initiating treatment when symptoms arise) is less effective. Approximately 60–70% of women with PMDD respond positively to SSRIs, with noticeable improvements within days (as opposed to the typical timeline seen in depression). In cases where SSRIs are difficult to tolerate or fail to yield results, it might be worth exploring a serotonin-norepinephrine reuptake inhibitor like venlafaxine, even if the supporting data is minimal. Anxiolytics (such as alprazolam) can be utilized temporarily for severe anxiety symptoms, and low-dose buspirone may assist with anxiety and irritability.
Struggling Alone?
North America Behavioral Health Services is here to assist you or your loved one in finding genuine support and solutions to your mental health concerns. Whether you’re dealing with anxiety, depression, trauma, or intricate mental health issues, we steer you towards the right facility, the right experts, and the most effective route to recovery.
Our network of reliable mental health professionals and treatment centers ensures that you won’t be traversing this journey without guidance.
Experience a healing journey that is:
✅ Confidential.
✅ Compassionate.
✅ Completely tailored to you.
Contact North America Behavioral Health Services today, because the right help can transform everything.
Begin the healing process.
















